
Understanding G6PD Deficiency
Not an Allergy, But Something Just as Important
By Dr Soo
When parents hear that their child has G6PD deficiency, one of the most common reactions is confusion and concern. Some may mistake it for an allergy, while others are unsure of what exactly it means. While G6PD deficiency is not an allergy, it is still a condition that requires awareness, careful management, and informed care.
Let’s break it down—what is G6PD deficiency, how does it affect your child, and most importantly, what should you do to keep your child safe and thriving?
What is G6PD Deficiency?
G6PD stands for glucose-6-phosphate dehydrogenase, an enzyme that plays a crucial role in protecting our red blood cells from damage. In children (and adults) who lack enough of this enzyme, certain exposures—such as specific foods, medications, and infections—can trigger the destruction of red blood cells, a condition known as hemolysis.
G6PD deficiency is one of the most common enzyme deficiencies worldwide, affecting over 400 million people. It is particularly prevalent in parts of Africa, the Middle East, Southeast Asia, and the Mediterranean. In Malaysia, G6PD deficiency is screened in newborns as part of the national health program, so parents are typically informed early if their baby has the condition.
Is G6PD Deficiency an Allergy?
This is one of the biggest misconceptions. No, G6PD deficiency is NOT an allergy. It is a genetic condition passed down through families, specifically through the X chromosome. That means boys are more commonly affected, while girls can be carriers.
Unlike allergies, which involve the immune system reacting to a substance, G6PD deficiency involves a lack of an enzyme in the red blood cells. The absence of this enzyme makes red blood cells more vulnerable to oxidative stress, leading to premature breakdown.
What Happens During a G6PD “Crisis”?
When a child with G6PD deficiency is exposed to certain triggers, red blood cells can break down rapidly. This can lead to acute hemolytic anemia, which may cause:
-
Pale or yellowish skin (jaundice)
-
Dark tea-colored urine
-
Extreme tiredness
-
Rapid heart rate or breathing
-
Poor feeding or irritability in infants
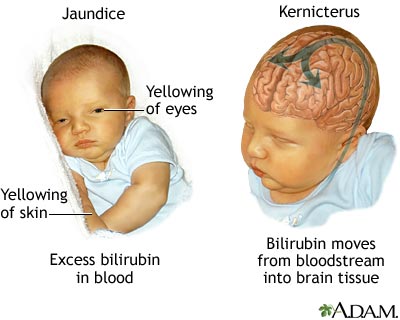
In newborns, severe jaundice may develop within the first few days of life and requires prompt medical attention to prevent complications such as kernicterus, a rare but serious form of brain damage caused by very high bilirubin levels.
What Are the Common Triggers?
Avoiding known triggers is the most important part of managing G6PD deficiency. Here are the main categories to be aware of:
Medications to Avoid
Certain medications are known to cause oxidative stress and should be avoided, including:
-
Antimalarials (e.g., primaquine)
-
Sulfonamides (e.g., sulfamethoxazole in cotrimoxazole)
-
Nitrofurantoin, dapsone, and chloramphenicol
-
High-dose aspirin and some NSAIDs (use only if approved by your doctor)
Always inform your doctor and pharmacist that your child has G6PD deficiency before giving any medicine.
Foods to Avoid
The most well-known food to avoid is fava beans (broad beans). Even small amounts can trigger severe hemolytic reactions in G6PD-deficient individuals.

Fava beans
Can Infections Be a Trigger?
Yes, infections can trigger a hemolytic episode in G6PD-deficient children. Even common viral illnesses can increase oxidative stress in the body. If your child becomes ill, especially with a fever, it’s important to monitor them closely for signs of hemolysis.
Your child’s pediatrician may recommend blood tests during or after an illness to assess their red blood cell count and overall health.
How to Live Safely with G6PD Deficiency
The good news is that most children with G6PD deficiency grow up healthy and active. Here’s how parents and caregivers can help ensure that:
Be Informed
Understanding the condition is your first line of defense. Share information with everyone involved in your child’s care, including teachers, babysitters, and relatives.
Inform Healthcare Providers
Always let medical professionals know about your child’s G6PD deficiency. Carrying a medical alert card or wearing a bracelet can be helpful, especially in emergencies.
Watch for Warning Signs
Be alert for symptoms such as dark urine, tiredness, or sudden paleness—especially during illness or after exposure to a trigger. Seek medical attention promptly if you observe any of these.
Use Medicines Wisely
Not all over-the-counter medications are safe. Paracetamol is generally okay, but consult your pediatrician before giving anything else. Avoid giving your child any medication without checking its safety for G6PD deficiency.
Is There a Cure for G6PD Deficiency?
There is no cure because G6PD deficiency is inherited. However, with good awareness and avoidance of triggers, children can lead full, active lives. In rare cases of severe anemia, a child may need a blood transfusion, but this is not common when the condition is well-managed.
Final Thoughts
G6PD deficiency may sound scary at first, but it doesn’t have to limit your child’s life. With awareness, support, and simple precautions, children with G6PD deficiency can grow, play, learn, and thrive just like any other child.
It’s not an allergy, but it does matter. Understanding what to avoid, what to look out for, and how to care for your child will make all the difference.
If you ever feel unsure or need guidance, our clinic is here to support you. Let’s work together to empower families, raise awareness, and help every child live their healthiest life.



